You might not be able to heal the injuries at all, or they may recover slowly. Diabetes can also affect circulation, which makes wounds more difficult to heal. Diabetic neuropathy can also affect wound healing.
Wounds that would typically heal within a few weeks can take months to heal in people with diabetes, leading to increased risks of infection and other complications. Wound healing can be a complex and challenging process for people with diabetes.
This blog post explores factors that affect wound healing in diabetes, the difficulties that can arise, as well as how to prevent and treat these issues.
How Does Diabetes Affect Wound Healing: 4 Factors

Let's discover the impact of diabetes on wound healing through these 4 crucial factors. Explore how this condition affects the body's ability to heal wounds and gain valuable insights into managing diabetes-related injuries effectively. Stay informed and take control of your health.
Levels of Blood Glucose
A high blood glucose level is a hallmark of diabetes and can have a detrimental effect on wound healing. When the body's glucose levels are too high, vital wound-healing processes are disrupted, making it more difficult to repair damaged tissue. Here are some ways elevated blood glucose levels impact wound healing:
- Reduced cellular proliferation: High glucose levels impair the growth and replication of cells involved in the wound-healing process, such as fibroblasts and endothelial cells.
- Impaired collagen production: The synthesis of collagen, a protein essential for wound healing, is also affected by high glucose levels, leading to a reduction in tensile strength and elasticity in the healing tissue.
- Increased inflammation: Elevated glucose levels trigger a pro-inflammatory response, increasing cytokines and inflammatory cells that can delay wound healing.
Poor Circulation
Diabetes can cause significant damage to blood vessels, leading to poor circulation and impairing the body's ability to deliver critical nutrients to the wound site. This can lead to the formation and worsening of diabetes-related foot ulcers. Here are some ways poor circulation affects wound healing:
- Reduced oxygen supply: Oxygen is essential for wound healing as it is necessary for the metabolic processes involved in tissue repair. Poor circulation can impede oxygen delivery to the wound site, leading to delayed healing.
- Impaired nutrient delivery: Adequate nutrient supply, such as minerals, vitamins, and amino acids, is crucial to wound healing. Poor circulation can minimize nutrient availability, delaying the healing process and increasing the likelihood of infection.
- Increased risk of infection: Poor circulation can make it harder for immune cells to reach the wound site, making individuals with diabetes more susceptible to infections.

Diabetic Neuropathy
Neuropathy, or nerve damage, is another common complication of diabetes that can have severe implications on wound healing. Neuropathy can reduce sensation, making it challenging to detect wounds, especially in the feet. Here are some ways neuropathy affects wound healing:
- Reduced ability to fight infections: Diabetes can weaken the immune response, reducing the body's ability to fight infections that can delay wound healing.
- Impaired cytokine response: Cytokines are crucial for the wound-healing process. Diabetes can alter cytokine production, delaying wound healing and increasing the risk of infection.
- Formation of biofilms: Biofilms are bacterial accumulations that can form around wounds. Diabetes can increase the risk of biofilm formation, making it harder for antibiotics to penetrate and treat infections.
Immune System Deficiency

Diabetes patients are more likely to contract infections due to an impaired immune response. The following are ways immune system deficiency can complicate wound healing:
- Reduced ability to fight infections:Diabetes can weaken the immune response, reducing the body's ability to fight infections that can delay wound healing.
- Impaired cytokine response: Cytokines are crucial for the wound-healing process. Diabetes can alter cytokine production, delaying wound healing and increasing the risk of infection.
- Formation of biofilms: Biofilms are bacterial accumulations that can form around wounds. Diabetes can increase the risk of biofilm formation, making it harder for antibiotics to penetrate and treat infections.
Diabetes on Wound Healing: The Complications
While it can lead to various health problems, one significant complication is impaired wound healing. Individuals with diabetes risk developing infections, delayed healing times, and associated complications more than those without diabetes. We will explore diabetic wound healing and discuss some practical tips to help manage this complication effectively.
Infection
Infection is a significant risk factor for individuals with diabetes. Here are some ways diabetes increases the risk of wound infections:
- Hyperglycemia impairs the immune system's ability to fight off infections, leaving individuals with diabetes more vulnerable to bacterial, fungal, and viral infections.
- Poor circulation, a common symptom of diabetes, reduces the flow of nutrients and oxygen to the wound, impairing the healing process and making it easier for bacteria to thrive.
- Diabetes can damage nerves, making it difficult to notice cuts, sores, or other injuries. This delay in detecting and treating wounds increases the risk of infection.
- It is common for diabetics to develop foot ulcers, which can become infected and result in amputations if not treated promptly.
Delayed Healing
Individuals with diabetes often experience prolonged healing times, resulting in higher healthcare costs. Here are some ways diabetes affects wound healing:
- Hyperglycemia interferes with collagen production, a protein necessary for wound healing. Thus, high blood sugar levels can impair the wound's ability to regenerate new tissue, leading to delayed healing.
- Poor circulation due to diabetes can cause ischemia, which means reduced blood flow to the wound. This hinders the delivery of vital nutrients and oxygen required for the wound to heal.
- Diabetes affects the function of white blood cells, causing them to become less effective in fighting infections, leading to an increased risk of delayed healing in wounds.
Diabetes Affects Wound Healing: Prevention and Treatment

We will address how diabetes affects wound healing and explore the various prevention and treatment options available.
Prevention
Preventing wounds in individuals with diabetes is crucial to avoiding complications. Here are some helpful tips to prevent wounds:
- Keep an eye out for cuts, blisters, and sores and attend to them promptly.
- Make sure your shoes fit well, and avoid wearing tight-fitting shoes or heels.
- Avoid walking barefoot or wearing sandals.
- Keep your blood sugar levels in control.
- Engage in physical activity every day to improve circulation.
Treatment
Treatment for wounds in individuals with diabetes can be complex and requires careful monitoring. Here are some effective treatment options:
- Wash the wound well with mild soap.
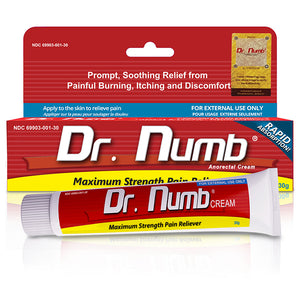
- Prevent infection by applying antibiotic ointment and covering it with a sterile bandage.
- Depending on the severity of the wound, it may be necessary to see a healthcare professional for further treatment, including debridement, dressings, and even surgery.
- Utilize compression therapy to improve circulation.
- Hyperbaric oxygen therapy may sometimes be necessary to promote wound healing.

Diabetes Management
Proper diabetes management is essential in preventing wound complications. Here are some tips for managing diabetes effectively:
- Monitor your blood sugar levels regularly.
- Follow a well-balanced, healthy diet.
- Exercise every day and aim for at least 30 minutes of exercise daily.
- Take medications as prescribed.
- Attend regular healthcare check-ups to monitor for any complications.
Conclusion
In conclusion, managing diabetic wounds can be challenging as this population is more susceptible to infections, delayed healing, and associated complications.
By understanding how diabetes affects wound healing, individuals can take proactive steps to maintain optimal blood sugar levels, improve circulation, practice proper wound care, and manage any associated complications.
Working closely with healthcare professionals and following best practices in wound care is critical for optimal wound healing outcomes.






![11 Types & 7 Benefits of Wound Ointments [Most Effective]](http://drnumb.com/cdn/shop/articles/What_Ointment_Is_Best_For_Wound_Healing__14_Types_7_Benefits.jpg?v=1716200317)